BackgroundTo improve transmural palliative care for older adults acutely admitted to hospital, the PalliSupport intervention, comprising an educational programme and transmural palliative care pathway, was developed. This care pathway involves timely identification of palliative care needs, advance care planning, multidisciplinary team meetings, warm handover, and follow-up home visits. With this study, we evaluate changes in patient-related outcomes and transmural collaboration after implementation of the care pathway.MethodsWe conducted a before-after study, in which we compared 1) unplanned hospital admission and death at place of preference and 2) transmural collaboration before implementation, up to six months, and six to 18 months after implementation. Data from palliative care team consultations were collected between February 2017 and February 2020 in a teaching hospital in the Netherlands.ResultsThe palliative care team held 711 first-time consultations. The number of consultation, as well as the number of consultations for patients with non-malignant diseases, and consultations for advance care planning increased after implementation. The implementation of the pathway had no statistically significant effect on unplanned hospitalization but associated positively with death at place of preference more than six months after implementation (during/shortly after adjusted OR: 2.12; 95% CI: 0.84–5.35; p-value: 0.11, long term after adjusted OR: 3.14; 95% CI: 1.49–6.62; p-value: 0.003). Effects on transmural collaboration showed that there were more warm handovers during/shortly after implementation, but not on long term. Primary care professionals attended multidisciplinary team meetings more often during and shortly after implementation, but did not more than six months after implementation.ConclusionsThe pathway did not affect unplanned hospital admissions, but more patients died at their place of preference after implementation. Implementation of the pathway increased attention to- and awareness for in-hospital palliative care, but did not improve transmural collaboration on long-term. For some patients, the hospital admissions might helped in facilitating death at place of preference.
MULTIFILE

Although Item Response Theory (IRT) has been recommended for helping advance interprofessional education (IPE) research, its use remains limited. This may be partly explained by potential misconceptions regarding IRT`s “limitation” to cross-sectional data. The aim of this study is to demonstrate how Item Response Theory (IRT) can be applied effectively in before-and-after designs in IPE research. Specifically, a two-week before-after design with survey methodology using the Extended Professional Identity Scale (EPIS), an interprofessional identity measure, was conducted among n = 146 mixed health-science students. Results indicated that EPIS increased significantly before-after intervention by.74 standardised mean differences, t146 = 7.73, p
DOCUMENT
ObjectiveWe designed a Patient and Family Participation Education Program (PFEP) with the aim of fostering a positive attitude and enhancing the competencies of hospital nurses required for effective patient and family participation in care.MethodsIn a Dutch university hospital, we conducted a before-after study. The PFEP comprising three courses: family conversation, supporting shared decision-making, and health literacy. We assessed nursing attitudes using the FINC-NA questionnaire and competencies with a separate questionnaire before and three months after the program. Changes in attitudes and competencies were analyzed using regression analysis.ResultsTwenty-two nurses participated in the education group, and 58 participated as controls.After three months, the change scores for the education group were statistically significantly higher on the total attitude score (FINC-NA) compared to the control group. Moreover, in six out of twelve competencies, the education group demonstrated significantly higher scores than the control group.ConclusionThe educational program appeared effective in promoting nurses' attitudes and feelings of competencies towards patient and family-centered care.InnovationA blended education program focusing on patient and family has potential value for implementation in hospital care settings, especially for hospitals aiming to cultivate a more patient- and family-centered environment.
DOCUMENT

OBJECTIVE: We designed a Patient and Family Participation Education Program (PFEP) with the aim of fostering a positive attitude and enhancing the competencies of hospital nurses required for effective patient and family participation in care.METHODS: In a Dutch university hospital, we conducted a before-after study. The PFEP comprising three courses: family conversation, supporting shared decision-making, and health literacy. We assessed nursing attitudes using the FINC-NA questionnaire and competencies with a separate questionnaire before and three months after the program. Changes in attitudes and competencies were analyzed using regression analysis.RESULTS: Twenty-two nurses participated in the education group, and 58 participated as controls.After three months, the change scores for the education group were statistically significantly higher on the total attitude score (FINC-NA) compared to the control group. Moreover, in six out of twelve competencies, the education group demonstrated significantly higher scores than the control group.CONCLUSION: The educational program appeared effective in promoting nurses' attitudes and feelings of competencies towards patient and family-centered care.INNOVATION: A blended education program focusing on patient and family has potential value for implementation in hospital care settings, especially for hospitals aiming to cultivate a more patient- and family-centered environment.
LINK
BACKGROUND: Medication-related problems are common after hospitalization, for example when changes in patients' medication regimens are accompanied by insufficient patient education, poor information transfer between healthcare providers, and inadequate follow-up post-discharge. We investigated the effect of a pharmacy-led transitional care program on the occurrence of medication-related problems four weeks post-discharge.METHODS: A prospective multi-center before-after study was conducted in six departments in total of two hospitals and 50 community pharmacies in the Netherlands. We tested a pharmacy-led program incorporating (i) usual care (medication reconciliation at hospital admission and discharge) combined with, (ii) teach-back at hospital discharge, (iii) improved transfer of medication information to primary healthcare providers and (iv) post-discharge home visit by the patient's own community pharmacist, compared with usual care alone. The difference in medication-related problems four weeks post-discharge, measured by means of a validated telephone-interview protocol, was the primary outcome. Multiple logistic regression analysis was used, adjusting for potential confounders after multiple imputation to deal with missing data.RESULTS: We included 234 (January-April 2016) and 222 (July-November 2016) patients in the usual care and intervention group, respectively. Complete data on the primary outcome was available for 400 patients. The proportion of patients with any medication-related problem was 65.9% (211/400) in the usual care group compared to 52.4% (189/400) in the intervention group (p = 0.01). After multiple imputation, the proportion of patients with any medication-related problem remained lower in the intervention group (unadjusted odds ratio 0.57; 95% CI 0.38-0.86, adjusted odds ratio 0.50; 95% CI 0.31-0.79).CONCLUSIONS: A pharmacy-led transitional care program reduced medication-related problems after discharge. Implementation research is needed to determine how best to embed these interventions in existing processes.
DOCUMENT

Background Physical activity after bariatric surgery is associated with sustained weight loss and improved quality of life. Some bariatric patients engage insufficiently in physical activity. The aim of this study was to examine whether and to what extent both physical activity and exercise cognitions have changed at one and two years post-surgery, and whether exercise cognitions predict physical activity. Methods Forty-two bariatric patients (38 women, 4 men; mean age 38 ± 8 years, mean body mass index prior to surgery 47 ± 6 kg/m²), filled out self-report instruments to examine physical activity and exercise cognitions pre- and post surgery. Results Moderate to large healthy changes in physical activity and exercise cognitions were observed after surgery. Perceiving less exercise benefits and having less confidence in exercising before surgery predicted less physical activity two years after surgery. High fear of injury one year after surgery predicted less physical activity two years after surgery. Conclusion After bariatric surgery, favorable changes in physical activity and exercise cognitions are observed. Our results suggest that targeting exercise cognitions before and after surgery might be relevant to improve physical activity.
MULTIFILE
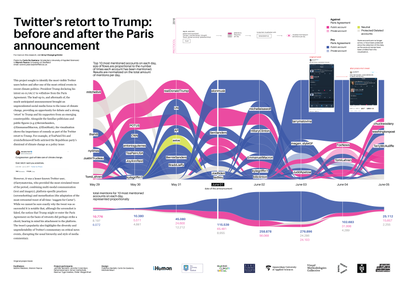
This project sought to identify the most visible Twitter users before and after one of the most critical events in recent climate politics: President Trump declaring his intent on 01/06/17 to withdraw from the Paris Agreement. The lead-up to, and aftermath of, the much-anticipated announcement brought an unprecedented social media focus to the issue of climate change, providing an opportunity for debate and a strong ‘retort’ to Trump and his supporters from an emerging counterpublic.
IMAGE
OBJECTIVE: Optimal timing of palatal repair is still subject of discussion. Although literature provides some evidence that palatal closure prior to 6 months positively influence speech outcome in children with clefts, only few studies verified this hypothesis. The purpose of this study was to describe and compare articulation and resonance characteristics following early (≤6 months) and later (>6 months) palatal repair, performed using the Sommerlad technique. METHODS: Comparison was made between 12 Ugandan children with isolated cleft (lip and) palate following early palatal repair (mean age: 3.3 m) and 12 Belgian patients with later palatal repair (mean age: 11.1 m), matched for cleft type, age and gender. A Ugandan and Belgian age- and gender-matched control group without clefts was included to control for language, culture and other environmental factors. Articulation assessments consisted of consonant inventories and phonetic and phonological analyses that were based on consensus transcriptions. In addition, resonance was evaluated by perceptual consensus ratings and objective mean nasalance values. RESULTS: The Belgian and Ugandan control groups were comparable for the majority of the variables. Comparison of cleft palate groups revealed no clinically relevant significant group differences for consonant inventory or phonological processes. Phonetic analysis showed significantly more distortions in the Belgian cleft palate group due to higher occurrence frequencies for (inter)dental productions of apico-alveolar consonants. Neither perceptual consensus ratings of hypernasality, hyponasality, cul-de-sac resonance and nasal emission/turbulence, nor objective mean nasalance values for oral speech samples revealed significant group differences (p>0.05). CONCLUSION: Articulation and resonance characteristics of young children following palatal repair before and after 6 months of age seem to be at least comparable.
DOCUMENT
Background: A new selective preventive spinal immobilization (PSI) protocol was introduced in the Netherlands. This may have led to an increase in non-immobilized spinal fractures (NISFs) and consequently adverse patient outcomes. Aim: A pilot study was conducted to describe the adverse patient outcomes in NISF of the PSI protocol change and assess the feasibility of a larger effect study. Methods: Retrospective comparative cohort pilot study including records of trauma patients with a presumed spinal injury who were presented at the emergency department of a level 2 trauma center by the emergency medical service (EMS). The pre-period 2013-2014 (strict PSI protocol), was compared to the post-period 2017-2018 (selective PSI protocol). Primary outcomes were the percentage of records with a NISF who had an adverse patient outcome such as neurological injuries and mortality before and after the protocol change. Secondary outcomes were the sample size calculation for a larger study and the feasibility of data collection. Results: 1,147 records were included; 442 pre-period, and 705 post-period. The NISF-prevalence was 10% (95% CI 7-16, n = 19) and 8% (95% CI 6-11, n = 33), respectively. In both periods, no neurological injuries or mortality due to NISF were found, by which calculating a sample size is impossible. Data collection showed to be feasible. Conclusions: No neurological injuries or mortality due to NISF were found in a strict and a selective PSI protocol. Therefore, a larger study is discouraged. Future studies should focus on which patients really profit from PSI and which patients do not.
DOCUMENT

BackgroundEarly structured mobilization has become a key element of Enhanced Recovery After Surgery programs to improve patient outcomes and decrease length of hospital stay. With the intention to assess and improve early mobilization levels, the 8-point ordinal John Hopkins Highest Level of Mobility (JH-HLM) scale was implemented at two gastrointestinal and oncological surgery wards in the Netherlands. After the implementation, however, healthcare professionals perceived a ceiling effect in assessing mobilization after gastrointestinal and oncological surgery. This study aimed to quantify this perceived ceiling effect, and aimed to determine if extending the JH-HLM scale with four additional response categories into the AMsterdam UMC EXtension of the JOhn HOpkins Highest Level of mObility (AMEXO) scale reduced this ceiling effect.MethodsAll patients who underwent gastrointestinal and oncological surgery and had a mobility score on the first postoperative day before (July–December 2018) or after (July–December 2019) extending the JH-HLM into the AMEXO scale were included. The primary outcome was the before-after difference in the percentage of ceiling effects on the first three postoperative days. Furthermore, the before-after changes and distributions in mobility scores were evaluated. Univariable and multivariable logistic regression analysis were used to assess these differences.Results Overall, 373 patients were included (JH-HLM n = 135; AMEXO n = 238). On the first postoperative day, 61 (45.2%) patients scored the highest possible mobility score before extending the JH-HLM into the AMEXO as compared to 4 (1.7%) patients after (OR = 0.021, CI = 0.007–0.059, p ConclusionsA substantial ceiling effect was present in assessing early mobilization in patients after gastrointestinal and oncological surgery using the JH-HLM. Extending the JH-HLM into the AMEXO scale decreased the ceiling effect significantly, making the tool more appropriate to assess early mobilization and set daily mobilization goals after gastrointestinal and oncological surgery.
MULTIFILE
